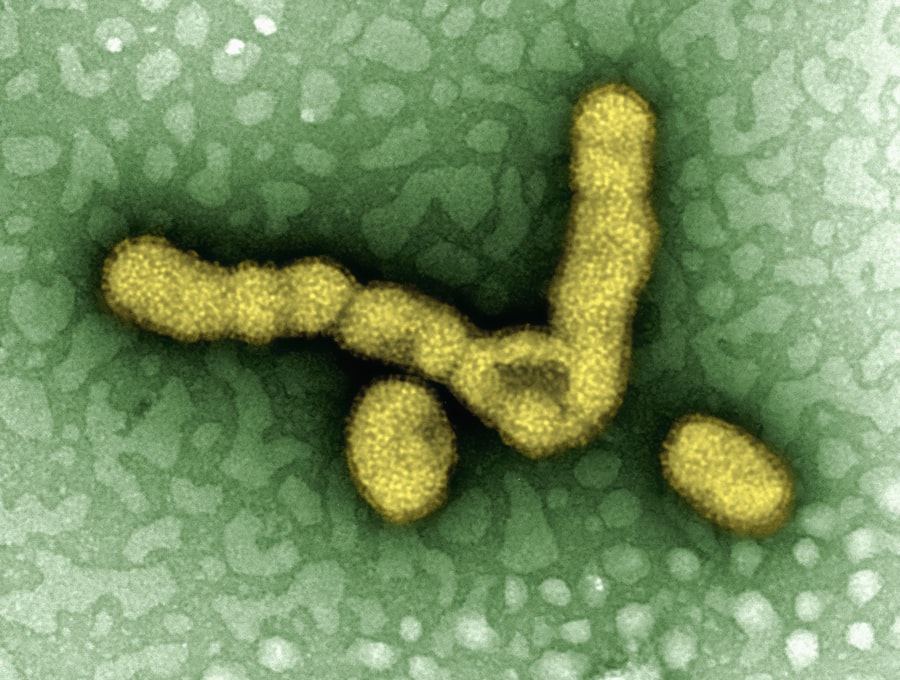
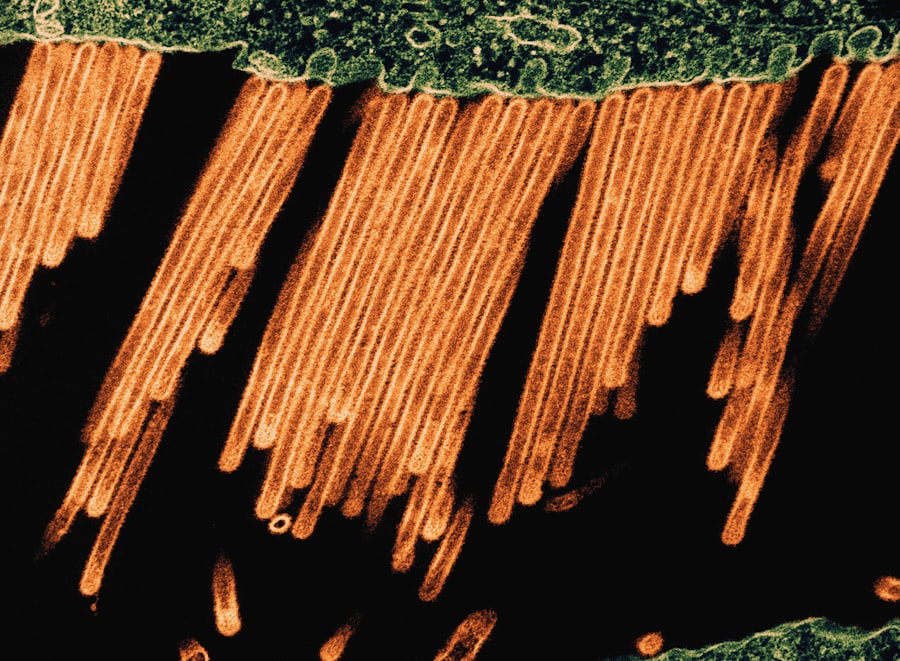
Influenza A is a subtype of the influenza virus that is responsible for seasonal flu epidemics and occasional pandemics. This virus is known for its ability to mutate rapidly, which allows it to evade the immune system and complicate vaccine development. Influenza A viruses are classified into various subtypes based on two surface proteins: hemagglutinin (H) and neuraminidase (N).
For instance, the H1N1 and H3N2 subtypes are among the most common strains that circulate in human populations. The World Health Organization (WHO) monitors these strains closely, as they can vary significantly from year to year, leading to variations in the effectiveness of vaccines. The transmission of Influenza A occurs primarily through respiratory droplets when an infected person coughs, sneezes, or talks.
The virus can also survive on surfaces for a limited time, contributing to its spread in crowded environments such as schools, workplaces, and public transportation. Understanding the nature of Influenza A is crucial for public health initiatives aimed at controlling outbreaks and minimizing the impact of seasonal flu on communities.
Key Takeaways
- Influenza A is a contagious respiratory virus with symptoms like fever, cough, and body aches.
- Preventive measures include vaccination, hand hygiene, and avoiding close contact with infected individuals.
- Treatment often involves antiviral medications and supportive care to alleviate symptoms.
- High-risk groups include young children, elderly adults, and individuals with weakened immune systems.
- Staying informed about vaccine updates and flu activity helps in effective prevention and management.
Symptoms of Influenza A
The symptoms of Influenza A can range from mild to severe and typically manifest suddenly. Common symptoms include fever, chills, cough, sore throat, runny or stuffy nose, muscle or body aches, headaches, and fatigue. Some individuals may also experience gastrointestinal symptoms such as nausea, vomiting, or diarrhea, although these are more prevalent in children than adults.
The onset of symptoms usually occurs one to four days after exposure to the virus, making it challenging to pinpoint the exact moment of infection. In many cases, individuals infected with Influenza A may initially mistake their symptoms for a common cold due to the overlap in symptoms. However, the intensity and rapid onset of flu symptoms often distinguish it from a cold.
For example, while a cold may develop gradually over several days, flu symptoms can escalate within hours. Additionally, the fever associated with Influenza A is typically higher than that seen with a cold, often reaching 101°F (38.3°C) or higher. Recognizing these differences is essential for timely diagnosis and treatment.
How to Prevent Influenza A
Preventing Influenza A involves a multifaceted approach that includes vaccination, good hygiene practices, and public health measures. The most effective way to prevent influenza infection is through annual vaccination. The flu vaccine is formulated each year based on predictions of which strains will be most prevalent during the upcoming flu season.
Vaccination not only protects the individual but also contributes to herd immunity, reducing the overall spread of the virus within communities. In addition to vaccination, practicing good hygiene is vital in preventing the transmission of Influenza Regular handwashing with soap and water for at least 20 seconds can significantly reduce the risk of infection. When soap and water are not available, alcohol-based hand sanitizers can serve as an effective alternative.
Furthermore, individuals should avoid close contact with sick individuals and stay home when feeling unwell to minimize the risk of spreading the virus. Covering coughs and sneezes with a tissue or elbow can also help contain respiratory droplets that may carry the virus.
Treatment for Influenza A
Treatment for Influenza A primarily focuses on alleviating symptoms and preventing complications. Antiviral medications such as oseltamivir (Tamiflu), zanamivir (Relenza), peramivir (Rapivab), and baloxavir marboxil (Xofluza) can be prescribed to reduce the severity and duration of illness if taken within the first 48 hours of symptom onset. These medications work by inhibiting viral replication, thereby helping the body mount an effective immune response against the infection.
In addition to antiviral medications, supportive care plays a crucial role in managing Influenza A symptoms. This includes staying hydrated by drinking plenty of fluids, resting to allow the body to recover, and using over-the-counter medications to relieve fever and body aches. In more severe cases or among high-risk individuals, hospitalization may be necessary for close monitoring and treatment of complications such as pneumonia or respiratory distress.
High-Risk Groups for Influenza A
| Metric | Value | Notes |
|---|---|---|
| Virus Type | Influenza A | One of the main types of influenza viruses causing seasonal flu |
| Subtypes | H1N1, H3N2, others | Based on hemagglutinin (H) and neuraminidase (N) proteins |
| Genome | Single-stranded RNA | Segmented into 8 parts |
| Incubation Period | 1-4 days | Time from exposure to symptom onset |
| Transmission | Respiratory droplets | Also via contact with contaminated surfaces |
| Symptoms | Fever, cough, sore throat, muscle aches | Typical flu symptoms |
| Annual Cases (Global) | 3-5 million severe cases | WHO estimate |
| Annual Deaths (Global) | 290,000-650,000 | Due to respiratory diseases linked to influenza |
| Vaccination | Seasonal flu vaccine | Updated annually to match circulating strains |
| Treatment | Antiviral drugs (e.g., oseltamivir) | Most effective when started early |
Certain populations are at a higher risk for severe illness from Influenza A due to underlying health conditions or age factors. Young children, particularly those under five years old, are more susceptible to complications from influenza due to their developing immune systems. Older adults aged 65 and above also face increased risks because their immune responses may be weaker or less effective against infections.
Individuals with chronic health conditions such as asthma, diabetes, heart disease, or weakened immune systems are also at heightened risk for severe influenza-related complications. Pregnant women are another group that requires special attention; hormonal changes and alterations in immune function during pregnancy can make them more vulnerable to severe illness from influenza. Public health campaigns often emphasize the importance of vaccination for these high-risk groups to mitigate potential health crises during flu season.
Complications of Influenza A
Influenza A can lead to a range of complications that may require medical intervention. One of the most common complications is pneumonia, which can occur when the influenza virus infects the lungs or when secondary bacterial infections take hold following an initial viral infection. Pneumonia can be particularly dangerous for high-risk groups and may necessitate hospitalization or even intensive care.
In rare cases, influenza can lead to more severe neurological complications such as encephalitis or myelitis. The risk of these complications underscores the importance of early recognition and treatment of influenza symptoms, especially in vulnerable populations.
Understanding the Influenza A Vaccine
The influenza vaccine is a critical tool in preventing Influenza A infections and mitigating their impact on public health. Each year, vaccine formulations are updated based on epidemiological data regarding circulating strains. The vaccine typically contains inactivated virus components or live attenuated viruses that stimulate an immune response without causing illness.
There are several types of vaccines available: trivalent vaccines protect against three strains (two A strains and one B strain), while quadrivalent vaccines offer protection against four strains (two A strains and two B strains). The effectiveness of the influenza vaccine can vary from year to year depending on how well the vaccine matches circulating strains. While it may not provide complete protection against infection, it significantly reduces the risk of severe illness and hospitalization among vaccinated individuals.
Public health authorities recommend annual vaccination for everyone aged six months and older, particularly for those in high-risk groups. Vaccination campaigns often coincide with the onset of flu season in order to maximize community immunity before widespread outbreaks occur.
Staying Informed and Prepared for Influenza A
Staying informed about Influenza A is essential for individuals and communities alike in order to effectively combat its spread and impact. Awareness of symptoms allows for prompt recognition and treatment, while understanding prevention strategies can help reduce transmission rates during peak flu seasons. Vaccination remains one of the most effective methods for protecting oneself and others from severe illness associated with Influenza A.
Public health initiatives play a vital role in disseminating information about influenza prevention and treatment options. By fostering a culture of awareness and preparedness, communities can better navigate the challenges posed by seasonal flu outbreaks. As research continues into more effective vaccines and treatments for Influenza A, maintaining vigilance through education and proactive health measures will remain crucial in safeguarding public health against this ever-evolving virus.
Influenza A is a significant strain of the flu virus that can lead to severe respiratory illness. Understanding its impact on health is crucial, especially during flu season. For those interested in maintaining their overall health and potentially boosting their immune system, a well-balanced diet plays a vital role. You might find it helpful to explore the nutritional benefits of various foods, such as those discussed in this article on top low-fiber vegetables, which can aid in digestion and overall wellness.
FAQs
What is Influenza A?
Influenza A is a type of virus that causes influenza, commonly known as the flu. It is one of the main types of influenza viruses that infect humans and animals, leading to seasonal flu outbreaks and occasional pandemics.
How is Influenza A transmitted?
Influenza A spreads primarily through respiratory droplets when an infected person coughs, sneezes, or talks. It can also spread by touching surfaces contaminated with the virus and then touching the mouth, nose, or eyes.
What are the symptoms of Influenza A infection?
Common symptoms include fever, cough, sore throat, runny or stuffy nose, muscle or body aches, headaches, fatigue, and sometimes vomiting and diarrhea, especially in children.
How is Influenza A diagnosed?
Diagnosis is typically based on clinical symptoms and can be confirmed with laboratory tests such as rapid influenza diagnostic tests (RIDTs), PCR tests, or viral culture.
What treatments are available for Influenza A?
Antiviral medications like oseltamivir (Tamiflu) and zanamivir (Relenza) can be prescribed to reduce the severity and duration of symptoms if taken early. Supportive care includes rest, hydration, and over-the-counter medications to relieve symptoms.
Can Influenza A be prevented?
Yes, prevention includes annual flu vaccination, practicing good hand hygiene, avoiding close contact with sick individuals, and covering coughs and sneezes.
What is the difference between Influenza A and Influenza B?
Influenza A viruses infect humans and many animal species and are responsible for most flu pandemics. Influenza B viruses primarily infect humans and usually cause less severe outbreaks. Both cause seasonal flu epidemics.
Are there different subtypes of Influenza A?
Yes, Influenza A viruses are classified into subtypes based on two surface proteins: hemagglutinin (H) and neuraminidase (N). Examples include H1N1 and H3N2, which are common in human infections.
Who is at higher risk for severe Influenza A infection?
High-risk groups include young children, elderly adults, pregnant women, and individuals with chronic health conditions such as asthma, diabetes, or weakened immune systems.
Can animals transmit Influenza A to humans?
Certain Influenza A viruses can be transmitted from animals, such as birds or pigs, to humans. These zoonotic infections can sometimes lead to new flu strains and potential pandemics.

